By Liberia Supply Chain Management Unit, VillageReach, and Last Mile Health
A global shortage of personal protective equipment (PPEs) is affecting health workers including Community Health Workers (CHWs) in low-income countries. These health and community workers are the frontlines of defence against infectious diseases including COVID-19 and need these PPEs to protect themselves before protecting the larger population. As first-line responders in the communities, CHWs are entitled to the same treatment for PPEs as nurses, doctors, and other health providers. Without PPEs, CHWs can neither maintain existing health services nor conduct the additional services required to control the spread of the COVID-19 virus.
Many countries have made commitments to integrate their CHW cadres into country primary health care networks in recent years. Realizing this commitment means integration in the planning and projections, including for COVID-19. This process of forecasting and planning for commodities is called a quantification exercise. During quantification, quantities and cost of products are estimated for a specific period and determined when shipments of the products should be delivered to ensure an optimal and uninterrupted supply.
As part of country-level rapid COVID-19 response efforts, VillageReach and Last Mile Health collaborated with the Liberian Ministry of Health’s Supply Chain Management Unit and other partners to develop a quantification process and tool for PPE. There are other great tools available now as well and no tool is one-size-fits-all. Although this particular tool is specific to Liberia, the tool, process, and its assumptions are broadly applicable to other countries. Below we highlight our findings, outline the steps we took and share a few lessons we learned along the way.
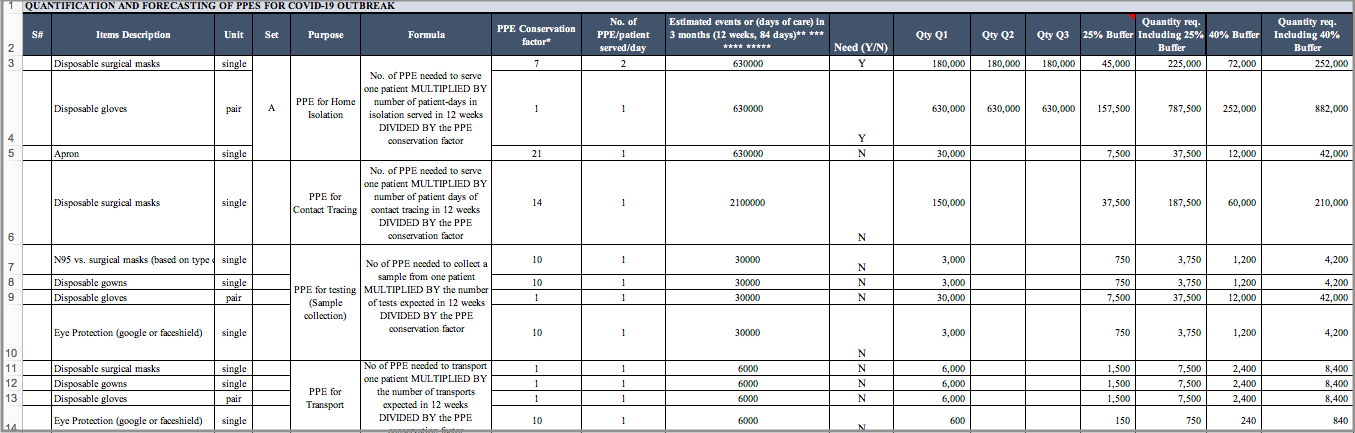
PPE Quantification and Forecasting Tool. Click to download .xls
What We Found
Community Health Assistants in Liberia serve 1.5 million people so their need for PPE is substantial. Since the government of Liberia has invested in the National Community Health Assistant (NCHA) Program, the stage was set for ensuring its 4,000 CHWs were included during quantification. VillageReach and Last Mile Health provided support to the Liberia Ministry of Health Supply Chain Management to estimate 1.08 million masks needed for health workers responding to COVID-19 over three months. Thirty-nine per cent (39%) of these quantified masks are expected to be allocated to CHWs who are also supporting patients and doing contact tracing at the community level. The Excel-based tool we developed here shows what’s needed for COVID-19 as well as routine services.
How We Got There
VillageReach and Last Mile Health moved into action to support the Liberia Ministry of Health based on its request during a COVID-19 coordination meeting. Six key steps we took over the course of a few weeks:
- Build the model: VillageReach and Last Mile Health adapted WHO guidance for essential resource planning to quickly quantify PPE needs as part of Liberia’s Coronavirus response strategy. After reviewing WHO guidance, we developed rules for calculating product needs at both health facilities and for Community Health Workers. This required collaboration between supply chain, clinical protocol, and government to adapt to our context.
- Make assumptions: We pooled our knowledge to link information about health products and services with national programs and policies. We made a series of assumptions and input them into the model such as plans for isolation centres, triage facilities at 600 health facilities, and the fact that CHWs are expected to do contact tracing and routine monitoring of COVID-19 in communities. We also built in recommended guidance, such as that a nurse can see seven cases with the same mask.
- Review assumptions: The Ministry of Health, VillageReach and Last Mile Health worked with National Public Health Institute of Liberia (NPHIL), WHO and UNICEF to review assumptions. We made changes based on evolving plans (e.g. number of isolation centres) and guidance (e.g. rationalizing the use of PPE, which is moderate compared with what was needed for Ebola.) There was pressure to include additional essential products, and we added some of them, such as reagents for testing.
- Address storage dependencies: We supported the Ministry of Health in determining the PPE storage needs at central and county level, as well as the county level planning and execution of distribution to free storage space for incoming supplies.
- Mobilize resources: We supported the Supply Chain Management Unit of MOH and NPHIL in further socializing the quantification with partners to activate procurement. This resulted in a request for a budget to support commodity procurement. UNICEF is using the forecast to procure PPE.
- Support procurement: We are now in the process of determining the procurement strategy (e.g. a mix of local vs international) and eliminating gaps in procurement where possible so that products are available nationally for health workers at the health facility and the community level.
Guidance for Others
Good Enough is Good Enough: Dispersed locations of key stakeholders lengthened the process and made it more challenging to reach alignment than if we were able to build consensus in person. An emergency requires a no-regrets approach to planning and decision-making like quantification. While imperfect, the process gave us valuable directional information to begin the procurement process. This model is being reviewed regularly and adapted as the situation on the ground changes.
Link Quantification to Other Processes: With quantification for PPE complete, the challenge turned to procure PPE. We realized that an emergency quantification process must be linked to an emergency procurement system. There is a big need for guidelines on how to adapt existing operational systems e.g. procurement SOPs, to suit requirements for emergency response procurement. Procurement continues to be a challenge and we took too long to find suppliers focusing on ‘verifying before buying’ (traditional approach) compared to ‘buying and verifying after,’ as we progressed. Some products are still in dangerously short supply and the suppliers are overwhelmed with orders placed earlier than ours. In addition to developing the quantification tool, we are developing a PPE inventory management dashboard that will show stock on hand and can be updated regularly as new stock and data come in. Combined, these tools will help the Liberian government and its partners optimize available resources and advocate for additional resources and equipment in the areas of greatest need.
Address Short-Term While Planning for the Future: Supply chain systems strengthening, and emergency response can and must happen at the same time. The crisis can help embed processes and capabilities in the system so that when the immediate needs are addressed, the government is more empowered post-crisis. We are already seeing how this will help optimize the supply chain for all products that CHWs need.
Nearly 1 out of 10 of Liberia’s health care workers lost their lives to Ebola, which continues to impact health care delivery today. We can’t afford to lose this race for PPE in Liberia, or anywhere.
Support for this work is funded by UBS Optimus Foundation and Skoll Foundation.





