In Ethiopia, non-communicable diseases are the leading cause of death. These illnesses—which include diabetes, cardiovascular disease, chronic respiratory diseases, cancers, kidney diseases, and others—account for 52% of deaths in the country.* And for those living in rural and remote communities, lifesaving screening and treatment is often out of reach at faraway hospitals: a costly journey that means many patients are unable to receive preventive or curative care until their condition has become dire.
Ethiopia’s flagship Health Extension Program, which trains and deploys more than 40,000 community health workers, has been critical in boosting maternal and child health outcomes and improving access to primary care. Facing the urgent need to address non-communicable diseases, the Ministry of Health added them to the Health Extension Program’s package of essential services in 2016. But by 2023, community health workers—nationally known as health extension workers—still had not received integrated in-service training on the topic.
“Imagine a scenario where community members can have their blood pressure or blood glucose measured at nearby health posts and also receive or be linked to appropriate treatments there. Imagine if these individuals also get informed on how they can protect themselves from infectious diseases,” says H.E. Dr. Derege Duguma, State Minister of Health with the Ministry of Health. “Taking immediate action is vital.”
Following the success of a new blended learning training for community health workers—an innovative approach including both digital and in-person learning, now being rolled out across the country—the Ministry and Last Mile Health began an ambitious new initiative: developing Ethiopia’s first integrated in-service training on non-communicable diseases for community health workers. The new training would use the blended model, which the Ministry has formally adopted for all community health worker training.
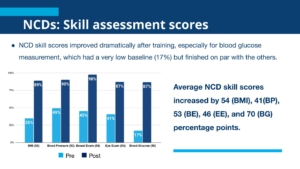
In January and February 2024, the first cohort of community health workers received training in non-communicable diseases as well as major communicable diseases. 273 community health workers and 27 supervisors from five woredas in Sidama and Southern Ethiopia completed training, participating in both in-person and digital sessions including video resources, applied skills practice, pre- and post-training knowledge and skills assessments, and resources available on their tablets for reference in the field or use with patients. Post-training assessments showed marked improvements in both skills and knowledge across topics. In practical skills assessments—critical to screening for and treating illnesses in the community—average scores for non-communicable diseases increased from 37% to 90%.
For community health workers, the impact of training is already tangible. “Before the training, we had limited knowledge about high blood pressure and diabetes mellitus, did not have a blood pressure apparatus, and did not give screening for these diseases. Most patients used to come after the diseases became worse when they reached a point where the diseases could not be treated. This would lead either to disability or death,” explains Zinash Bogale, a community health worker at Hida Kality Health Post. “We are now doing early identification and heading home with good news.”
Patients, too, are already experiencing improved access to services. “I have been told to do a blood test today at the health post. Now, I have been diagnosed with high blood pressure, and they gave me a counseling service on how to control it,” shares Tilahun Dudura, a community member in Hida Kality kebele. “I am happy to have this quality service near my home without any financial burden. The health post is like our home.”
Last Mile Health and the Ministry of Health have applied adjustments to the training based on initial results and shared the results at an event bringing together community health workers, Ministry staff, donors, and other key stakeholders. Already, scaling of the training has begun. “We have trained a small fraction from the 40,000 community health workers we have,” says Melaku Yilma, a capacity-building expert with the Health Extension Program. “But unless we train all the health extension workers in the country, we can’t expect to achieve our targets. We have to work together to build a system to guarantee these trainings are given and that all the critical equipment they need to provide the services are available at their health posts.”

Abraham Zerihun Megentta presents findings from the pilot training at the dissemination event in March 2024.
Ethiopia’s community health program is considered a global exemplar—and Last Mile Health and the Ministry of Health hope the new training can provide valuable lessons for other national programs to implement similar trainings. “We believe the Health Extension Program, by capitalizing on its past experience, can play a significant role in the fight against non-communicable diseases,” says Abraham Zerihun Megentta, Last Mile Health’s Ethiopia Country Director. “Non-communicable diseases are becoming huge burdens to Ethiopia and many other African countries, and in order to reach the vast majority of the population, we believe community health programs will play a crucial role.”
*Source: WHO.