Building an evidence base in recruitment, training, and implementation
In 2021, Last Mile Health and the Sierra Leone Ministry of Health embarked on an ambitious research initiative: examining the recruitment, training, and implementation of the country’s first fully-integrated community health worker program. Supported by Exemplars in Global Health—a program that identifies positive outliers, studies successes, and shares findings for adaptation—Last Mile Health’s initiative in Sierra Leone aimed to contribute to the global evidence base for strong community health worker programs as a driver of universal health coverage and improved health outcomes in rural and remote communities. “If we’re to achieve universal health coverage, community health workers are an integral part,” says Dr. Brima Osaio Kamara, Director of Sierra Leone’s Directorate of Primary Health Care. “The ministry is actively moving forward data for decision-making. We cannot achieve this if the quality of the data is poor.”
To gather, analyze, and leverage quality data on Sierra Leone’s community health worker program, Last Mile Health’s research consisted of four key objectives:
- Evaluate variation in community health worker recruitment outcomes and assess quality of district-level training to anticipate implementation support needs and improve future trainings
- Establish replicable community health program systems, equipping the Ministry of Health to make rapid operational and programmatic improvements
- Use data to identify challenges and inform quality improvements within the Sierra Leone National Community Health Worker Program
- Share lessons learned with a global audience and use data to advocate for additional funding for Sierra Leone’s community health worker program
In its first phase, Last Mile Health’s research gathered demographics and training data for a new cohort of 8,000+ community health workers, with results disseminated nationally in August 2023. (Learn more about the research and findings in this blog post.) Next, the team embarked on the second phase of research: studying the implementation of the national program.
Evaluating community health worker program implementation—as it happens
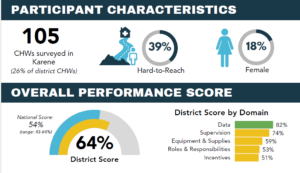
In the second phase of the research initiative, Last Mile Health studied the implementation of the national program across all 16 districts in the country. The team conducted phone surveys of community health workers; conducted key informant interviews with peer supervisors and district-level health leaders; and reviewed records such as supply logs, payment records, and patient reports. The research team sought to understand the overall performance of the program: are community health workers delivering the healthcare services they are supposed to be delivering; are they receiving appropriate supplies, supervision, salaries, and reporting tools; and are they regularly sharing data?
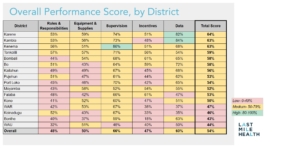
The team also examined data to understand differences across demographics—including district by district; hard-to-reach versus easy-to-reach communities; and the gender, age, experience, and education level of community health workers. Finally, they aimed to understand the implications of the data regarding the status of program implementation and potential areas of strength or challenge, district by district—and how learnings could lead to a light-touch, low-cost performance monitoring system for the Ministry of Health to track the program’s progress.
A key feature of the research, explains Last Mile Health’s Sierra Leone Country Director Christina Bowles, is its real-time evaluation of a new program. “This is implementation science,” she says. “Research often looks back in time, but this is a process evaluation. We’re backing up a step: not focusing on program impact, but focusing on the process.” The research is national in scope, with each of Sierra Leone’s 16 districts facing its own challenges in environment, disease burden, and percentage of hard-to-reach communities. “There are interventions we can make at the national level to improve quality, but also interventions within each district that show solutions from that district individually—interventions that apply to their districts and address their unique needs,” says Christina. This means the research gathers data and builds recommendations both for national-level policy and district-level implementation.
Sharing findings with district-level stakeholders to develop improvements together
In June 2024, Last Mile Health and the Ministry of Health completed a series of subnational dissemination events, sharing research results and identifying opportunities for improvement with district-level stakeholders. Participants from every level of the health system—community health workers, peer supervisors, district-level health leaders, and national-level Ministry staff—reviewed district-specific reports, shared challenges and successes, and worked to develop action plans and recommendations.
Karene, a district in North West Province, serves as an example of district-level results and recommendations. Overall, the district performed well: 100% of surveyed community health workers reported that their community health registers for data reporting were in stock, 88% reported receiving a supervision visit within the last month, and 99% reported that they had provided antenatal household visits and routine household visits during the survey period. Still, a number of indicators showed room for improvement—from inconsistencies in the timing and amount of pay incentives received to widespread stock-outs of essential supplies.
At Karene’s subnational dissemination event, stakeholders dug into the challenges community health workers faced on a deeper, detailed level. Participants identified solutions to the challenges the research results revealed, developing recommendations that included stronger monitoring of immunization status during patient visits to primary health facilities, creating separate tracking booklets to boost malnutrition screenings, and increasing supervision for primary health facility staff and district focal staff.
At the end of each dissemination event, district stakeholders came away with a clearer understanding of where they could improve the implementation of the national program in their districts—and a concrete set of recommendations and plans. In turn, these recommendations will inform the national dissemination of the Exemplars research in August 2024, as Last Mile Health works in partnership with the Ministry of Health to develop national-level recommendations for better implementation of the program. National- and district-level work will continue in this ongoing loop, with national policy informing district practice, and district recommendations informing adjustments to policy and recommendations for its implementation.
Next steps: Sharing results nationally and globally to improve program implementation
Ultimately, Last Mile Health will disseminate the results of this research globally to share lessons learned with other governments and partners in the early stages of implementing national community health worker programs. The recommendations and insights shared during the subnational disseminations will be key—and critically, they will include perspectives from every level of the health system, including community health workers. Despite a growing global understanding that community health workers must be represented in decision-making on community health programs—a condition for which Last Mile Health has long advocated—this is rarely the reality. The findings from our research in Sierra Leone represents a step forward in ensuring those closest to the work contribute to policy and practice.